The Innate Immune system
The Innate immune system is the inherited immune system that is based upon recognizing the core unchanging features of infections.
Your skin's epithelial and fibroblast cells are the first line of defense agains foreign infections.
After the skin barrier protection is broken the sentinel macrophage greets the visitor. Macrophages do not travel to the lymph but kill the foreign infections engulfing them like a pac-man and alert the rest of the immune system. The LPS of a bacteria stimulates the macrophage to become active and produce il-6 which signals the creation of the innate immune system army.
il-6 stimulates the production of Neutrophils, Mast cells, Basophils, Eosinophils, and more monocytes. Monocytes can develop into macrophages or dendritic cells.
Here is a quick summary of the innate's immune system army:
Macrophages which are the immune system's sentinels. Macrophages kill and alert of foreign infections of any kind.
Neutrophils are specialized to destroy and consume bacteria. Neutrophils throw down nets to trap infections in an area.
Mast cells help to identify if it is a viral or bacterial infection then release histamine to bring more immune system cells to the area, the next adaptive immune system. Skin derived mast cells taste through endocytosis the infected area for viruses. While TLR butterfly nets on the surface of bone derived mast cells look for bacteria.
Eosinophils help to breakdown extremely large infections into smaller bite size pieces for neutrophils.
Basophils Like mast cells there are 2 types. Basophils aid in attacking infections like mycobacterias by releasing heparin and serotonin while a second type aids in the viral attack. The duty of Basophils are to help mast cells transition the immune system from innate to adaptive but Basophils have a special relationship as a liaison to TH2. (
Basophils appear to create the il-4 burst which develops the TH2 cells from TH0 and they can antigen present to TH2 cells which will be covered in the Adaptive Immune system)
How does the Innate immune system start?
For invading bacteria our immune system has evolved an attack based on the standard surfaces of the bacteria. There are three basic bacterial surfaces: flat and reachable, mannose sugar covered and semi-reachable and completely covered unreachable surfaces. The flat surface of something like staph can be dealt with through an antibody binding pathways called
Complement. The long mannose sugar strand covered type of bacteria's like strep are dealt with using a
Mannose Lectin pathway. The bacterias like e.coli that have so much surface junk that nothing can be built on the surface are dealt with using an
Alternative pathway. In attacking the surface of the bacteria there are two goals. To place gripper receptors for phagocytosis by macrophages or neutrophils on the bacteria or to create a "membrane attack complex" which forms a pore into the bacteria which leaks the guts of the bacteria out thus killing it.
The Complement Pathway
Macrophages which are the sentinels of the immune system have TLR sensors. These TLR sensors are butterfly net type of attachments that when triggered stimulate the macrophage to produce il-6. il-6 cytokines are messages sent to tell B cells to make the generic simple IgM antibodies. This IgM pentagon antibody with it's 5 legs easily bind foreign objects in a non specific way. The FC portion of the antibody interacts with complement proteins to slowly create the phagocytosis handles and the MAC pore.
The Mannose-Lectin Pathway
This pathway involves sticking to long sucrose hairs and then slowly dropping the phagocytosis handles and MAC pore pieces down onto the surface and the bacteria is killed.
The alternative pathway
Because nothing can be built upon the surface the MAC pore is assembled off the surface and then plunged in as one giant unit. (no phagocytosis handles can really been seen on this surface)
The Adaptive Immune system
This is the stage where the immune system adapts to an infection and creates antibodies which bind specifically. This is not inherited this is created based on current environment exposure. First they must not recognize self antigens. B cells are educated in the bone marrow to not recognize outer self antigens. T cells are educated in the thymus to not recognize self antigens inside host cells. The receptors produced from these educations should only bind foreign matter.
There are four major immune system areas: the lymph glands, the spleen, the peyer patches, and the omentum milky spots. Lymph glands are responsible for lymph fluid, peripheral tissue, and surface infections. The spleen monitors the blood. The peyer patches monitor the mucosal membranes of the intestine through M cells. The Omentum's milky spots are lymph like glands that monitor the abdomen specifically the transition of nutrients from the intestine to the blood stream.
B1 cells of the omentum are the primary source of IgM and are the primary producer of the monomer form of IgA in response to il-5.
Langerhans carry antigens to the lymph glands' follicular dendritic dells.
Marginal Zone B cells are the spleen's version of langerhans.
Myeloid and plasmocytioid dendritic dells have evolved like macrophages from myeloid (bone marrow) cells but they do not appear with the innate system and like Langerhan cells they are antigen presenting cells for foreign antigens found inside of cells.
B cells are the antibody producing cells of the immune system. Their B cell receptors are educated in the bone marrow to know outer self antigens and react only to foreign outer antigens.
T Cells are the coordinator of what type of antibody to make. Different T cells are assigned to different zones. They look at the antigen presenting cells then secrete the correct cytokine to the B cells. The T cells are educated to know the self antigens of the inside and the T cell receptor when only react when binding an unknown antigen from inside the infected cell.
The follicular dendritic cell, which are starfish-like shaped cells, present antigens to a B cell. B cells use a membrane bound antibody called a BCR ( b cell receptor ) to bind the antigen. This B cell undergoes somatic hypermutation of the BCR until the binding is strong enough to remove the antigen from the dendritic cell and pull it into the B cell. The B cell then processes the antigen and acts as an antigen presented to T follicular cells. The T follicular cells then stimulate the B cells to make antibodies. Note that these B cells that were already active making IgM and must go through somatic switching to the IgA, IgE or IgG1.
When it is a viral infection macrophages or skin derived mast cells find they call myeloid and plasmacytoid dendritic cells to the area. Dendritic cells taste the area then travel to lymph glands where they act as antigen presenting cells to T cells. When the TCR (T cell receptor) of the T cell identifies a non self DNA or RNA segment it then interacts with a B cell stimulating it to produce antibodies. In summary, there are three distinct antigen zones that the immune system focuses on: the outer antigens, the cytosol antigens, and the nuclear/mitochondrial antigens.
All of these are T follicular cells but the Tfh comes from Th2.
the Tc follicular
virus: HIV have TFH cells with: pd-1 icos cd40 and cxcr5 : il-10
http://www.jimmunol.org/content/jimmunol/early/2016/07/30/jimmunol.1600143.full.pdf?with-ds=yes
the TH1 follicular
influenza TFH: pd-1, icos cxcr3. cxcr5 : ifn gamma and il-2
https://www.ncbi.nlm.nih.gov/pubmed/27231124
https://www.ncbi.nlm.nih.gov/pubmed/23486778
The starfish shape is the FDC cell showing the B cell the antigen.
The CD4 and CD8 act as clips holding the MHC mailboxes for the T cell to look in with their TCR. CD4 clips are on Tfollicular helper cells and Thelper cells while CD8 are on the TC cells. The MHC1 mailboxes which includes HLA-A of the nucleus and HLA-B of the mitochondria hold up viral nucleotide antigens. The MHC2 which includes HLA-dr and HLA-dq hold up antigens of the cytosol.
Note that Chlamydia as a bacteria gives rise to IgG3. Why would a bacteria give rise to IgG3? Chlamydia is named for the greek word Khlymus which means cloak. Chlamydia wraps around the nucleus of the cell it infects.
While IgG3 is known to bind viruses that infect the nucleus or mitochondria. (HIV vaccine that was 30% protection was due to increased IgG3 antibodies)
The TH17 linked bacteria and parasites may be linked to IgG3 antibodies. (under consideration right now)
The outer antigen B cell is the one that goes through somatic hypermutation improving the binding of the antibody. The isotype of the antibody made the B cell changes based on the hormone of the area. The spleen which grows into the pancreas would see high levels of insulin. The intestine which is in a constant state of replacement exposes the peyer patches to high levels of growth hormone. While your skin and the lymphs close to them would see high levels of insulin like growth factor which is involved with the development of new skin cells. The hormones of each of these areas dictates the isotype of the antibody. The B cells will make IgE at the lymph glands, IgA at the peyer patches, and IgG1 at the spleen. The exception to this is when a parasite triggers il-5 which triggers the monomer form of IgA. Normally only the dimer form of IgA is produced which in the intestine aids in the clumping and disposal of infections where the clumps are washed away. Parasites like worms tend to be larger and can not be clumped and washed away rather they need to be broken down.
The B cells of of the outer region first make IgM after il-6 exposure then class-switch to IgE or IgG1 or IgA. The B cells of the inner regions, the cytosol or mitochondrial/nuclear regions, do not make IgM first but are triggered by il-3 exposure.
In addition to the start cytokines il-3 or il-6 the B cells need to be activated by ICOS an inducible co-stimulatory molecule, il-21, and a cytokine that informs it of the region IgG region. T cells only express icos after cd28/pd-1 and TCR stimulation.
The above diagram is missing the T cell activation B7 receptors. For simplicity I have removed the CD4 and CD8 clips and focused on them.
The B7-h1 inhibits while the others stimulate...perhaps because you don't want CTLs to be fast to choose to kill. As pd-1 expression goes down with TCR stimulation on the Tc activation increases?
IgG3 increase x3 in pd-1 negative mice
https://www.ncbi.nlm.nih.gov/pubmed/9796923
For large visible infections il-6 stimulates B cells but for viral infections it is the skin derived mast cells that turn the B cells on with il-3.
MHCs are the mailboxes that hold up antigens for T cells aka HLAs. If you look at viral infections the the mailboxes that are associated with them you see this pattern. HLA-D covers infections in the cytosol and infections outside of the cell probably because so many infections when given a chance move inward hiding in the host.
So the butterlfy-net TLRs carried by macrophages and dendritic cells when triggered release different IFNs which then triggers the expression of the correct HLA mailbox. The matter that had been taken up by endocytosis, which tagged the TLRs is then processed in dendritic cells and held in the correct HLA mailbox. Myeloid Dendritic cells work with cytosolic antigens. Plasmacytoid dendritic cells work with the nuclear or mitochondrial antigens.
Note that IFNgamma is special in that it is a cytokine for all infections not in the nucleus or mitochondria and is used by the TH1 cells to mean an infection in the Cytosol region. This may have evolved because if the ER is compromised than nothing reaches the surface of the infected cell and they are easy to identify as problematic.
When a host cell has viral infections of the ER no proteins reach the surface of the cell and the host cell becomes naked. When NK's KIR binds to HLAs it knows the cell is healthy and won't attack. When a cell has no HLAs to bind the KIR the NKis triggered to attack.
il-3 sends the nk on the viral pathway while il-6 sends the NK on the bacteria pathway for something hiding in the cytosol of cells.
Specialty cells:
TH9 cells are for Cancer cells. When a tumor triggers il-4 but no il-5 varifies the presence of a bacteria and TGF-b1 notifies of a nuclear virus then TH9 cells are created. il-9 is a cytokine that has been found to suppress tumor growth and then il-21 helps to trigger Th17 cells.
TH17 cells are for second poppings. If a bacteria has moved inside of a vacuole or inside of the golgi then it needs to be popped out. The same is true for viral infections of the nucleus and mitochondria.
maybe? TGF type helps?
Note that the TH17 cell hypothesis still needs to be proven,
Another hypothesis that needs proving is how the cytosol viruses are seen by the IgG2 antibodies using 25HC.
The CTLs function differently in the inner regions. Il-2 stimulates Fas ligand killing. Fas expression in cytosol infected cells. il-21 increases killing through Tcr stimulation.
Note that there are 3 ways for cells to die. Necrosis which is premature death due to injury, pyroptosis which is programmed death due to an infection and then apoptosis which is a programmed cell death through the mitochondria which the cell can choose to do in old age.
Granzyme A and inflammazones create il-1b which trigger pyroptosis. Granzyme B triggers apoptosis.
The Gamma delta T cells and the NKT cells work together to produce antibodies against lipids. (hypothesis) Note here is where somatic hypermutation would occur for the viral lipid antigens. The invariant form would involve the myeloid dendritic cell's cytosol lipid antigens and the outer visible lipid antigens picked up B cells.
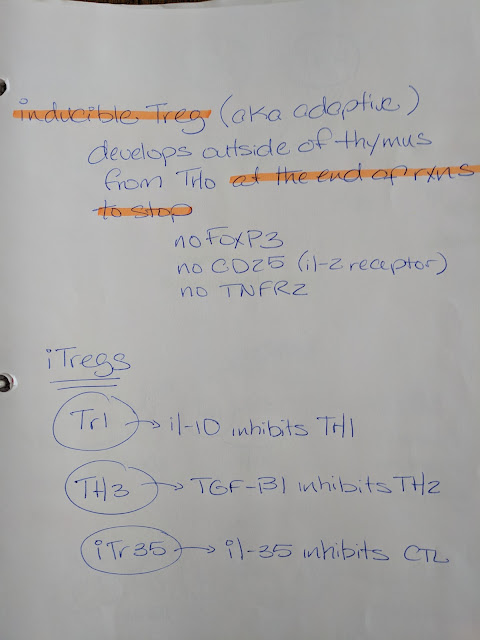
Natural T regulatory cells are used to focus the immune system and then inducible T regulatory cells stop the process at the end. I say CTL but it should be the Tc pathway.
The B7 receptors patterns could also tell the cells when to become T regulatory cells (hypothesis)
Chemokines are involved with the migration of immune system cells. The three antigen zones become apparent when organizing the chemokine receptors.
Chemokine receptors also link the immune system cells to the correct immune system gland.
What happens when bacteria or parasites are hiding in the cytosol ?
The Basophils create the TH2 that secrete il-13.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5293035/
Basophils are the bridge back to the outer antigens pathway. Trogocytosis involves the transfer of plasma membrane between antigen presenting cells and other immune system cells so that they may express the surface molecules specifically antigens in MHC2 on their own surface. In this case the myeloid dendritic cell is expressing an antigen that is a forein protein in the MHC2. By transferring this to the Basophil the correct immune system pathways will be triggered. The newly formed TH2 secreting il-13 informs the eosinophils that the infection is in the cytosol of infected cells.
il-13 functions similar to il-4 however il-13 suppresses apoptosis. Infections are held by the myeloid dendritic cells' MHC2 and trigger the il-2 CTL which use Fas to trigger apoptosis in infected cells.
Eosinophils, monocytes, and neutrophils all have fas which allows for the halting of inflammation of this pathway quickly but if they have seen il-13 which they also have a receptor for they will not go through apoptosis. This means that when a bacteria or parasite has moved into the cytosol the CTL with its Fas ligand will kill only the infected cells. When the neutrophils, eosinophils, or monocytes see the parasite released from the cytosol of the apoptosis infected cell the parasite can be exterminated. Only when the il-13 exposure wears off can the phagocytes again be triggered by fas themselves.
How are cytosolic viruses seen and killed? CTL fas ligand cells kill the infected cells through fas or 25hc which is released by activated macrophages. 25HC is only grabbing cytosolic viruses because it can't see the viruses in the nucleus or the mitochondria. The cytosolic viruses are held outside of the infected cell and the IgG2 antibodies are able to interact with them there and set off an innane system pore to kill infected cells.
While cytosolic viruses burst through the plasma membrane the nuclear and mitochondrial viruses use membrane budding, 25HC blocks nuclear and mitochondrial viruses by changing the plasma membranes. Only when theses inner viruses go through the golgi does 25HC then try to stop them by changing the cholesterol fluidity of the plasma membrane so the enveloped viruses can't bud.
What about exosomes? They deliver what is in cells, specifically infected or stressed cells, to dendritic cells
Exosomes may also be involved in Tolerance.
Tolerance is the "self education" given the B and T cells. B cells have been taught the external antigens in the bone marrow while T cells have learned the internal DNA/RNA antigens in the thymus. These self educations where all genes are expressed are called Central Tolerance.
Peripheral Tolerance is given to B and T cells by the gatekeeper cells of the lymph glands: the Lymphatic Endothelial cells. Lymphatic endothelial cells express the tissue specific genes of the cells of their area. They also sample and wear the antigens commonly found in their area.
These lymphatic endothelial cells will only allow in T and B cells that do not react with the self antigens specific to the tissues of the of the peripheral area into the lymph gland. (B cells are hypothesized to be educated too but this is not proven)
Current ideology is that if we can get antigens from a transplanted organ into the LEC tolerance to the transplanted organ will occur. The question is how is this done exactly and how often do LEC update their antigens.
Over simplified FC receptors and antibody relationship
Fc gamma : IgG
Fc epsilon: IgE (phagocytosis or degranulation)
Fc alpha: IgM , IgA eosinophil degranulation or IgA neutrophil nets
The dimer of IgA has no FC exposed to bind and has the ability to cross the mucosal membrane.
The hormone connection of antibodies can also be seen with the GSMD pores. Why ? Does the core of the pore match up with the pore of the middle of the antibody?
IgE at the skin's
IGF-1 with the GSDMA pore?
IgA ,
GH with GSDMB ?
IgG1,
insulin with GSDMC ?
The GSDM is made by the caspase-1 of inflammasomes. There are 2 major types of inflammasomes.
Both can end in either apoptosis or pyroptosis based on the type of infection that started them.
When cytosol infections trigger apoptosis there is the option of pyroptosis. Viral infections favor apoptosis while parasitic cytosol infections favor pyroptosis. As suggested above the GSDM pore created may function as a window for esosinophils to see the parasite inside.
Apoptosis can occur from DNA damage triggering p53 or from the triggering of FAS which turns oh the Death inducing domain leading to caspase. (DISC) In these cases no pyroptosis can occur.
Apoptosis: